KEYS POINTS
- Physical activity as a therapeutic tool in physiotherapy does not show a significant difference in the quality of life of patients undergoing bariatric surgery.
- It is important to consider that this review presents a high level of heterogeneity due to the diversity of physical activity programs, the different time points of measurement, and the various quality of life assessment scales. Moreover, the nature of trials involving non-pharmacological interventions inherently includes a bias due to the inability to implement double blinding.
- Nevertheless, there are no contraindications against physical activity, as it carries very little risk and no side effects. However, to achieve an optimal effect on patients’ quality of life, a multidisciplinary approach is necessary. It should integrate physical activity, psychological support, and dietary counselling simultaneously.
- The physiotherapist’s role in this care pathway remains essential. Their involvement helps guide the patient through post-surgical physical adaptations and allows for a personalized approach. This should include active listening and a therapeutic education process to enhance patient adherence and promote an overall improvement in quality of life.
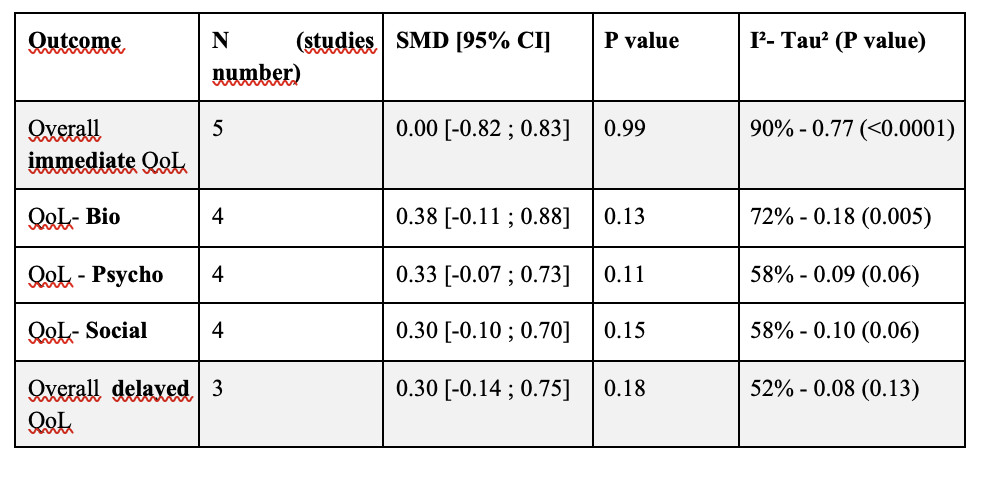
RESULTS
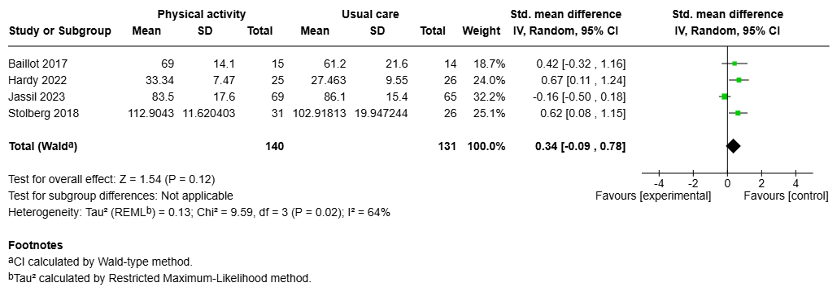
1. Overall immediate post-intervention analysis
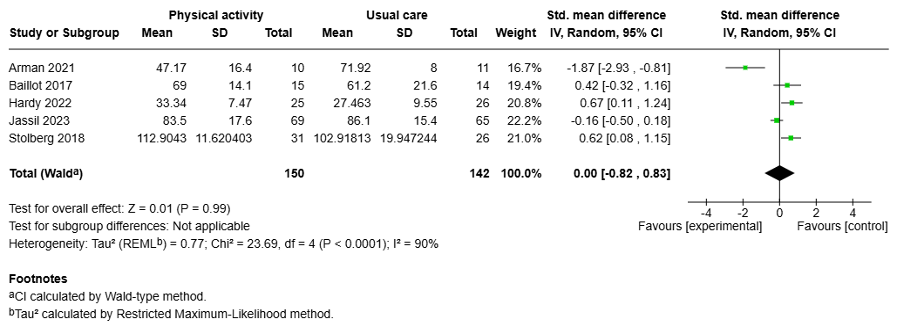
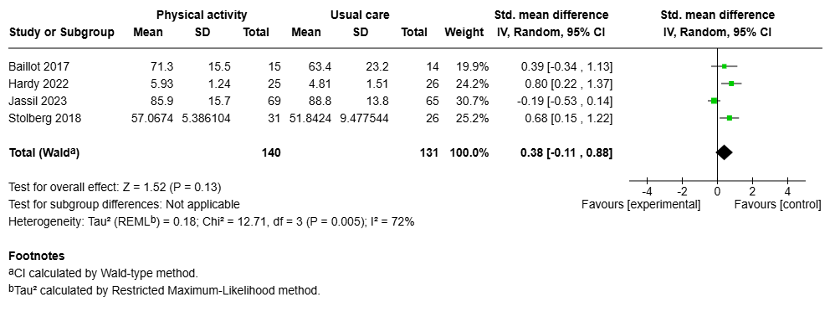
2.Overall immediate post-intervention analysis (after sensitivity analysis)
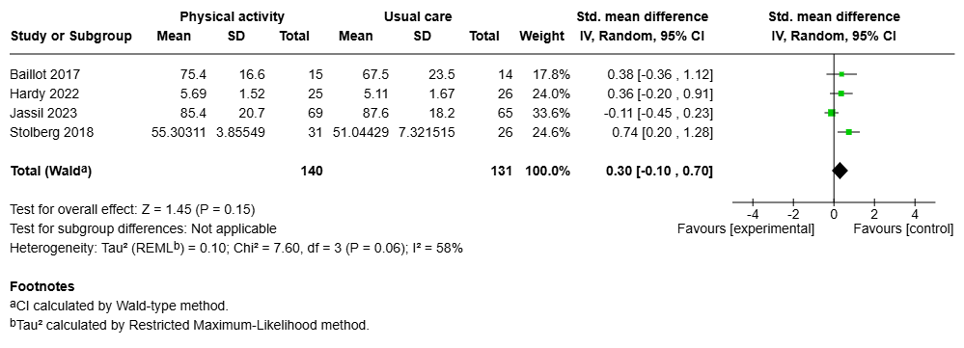
3.Bio-psycho-social subgroups analysis
3.1.Biological domain
3.2.Psychological domain
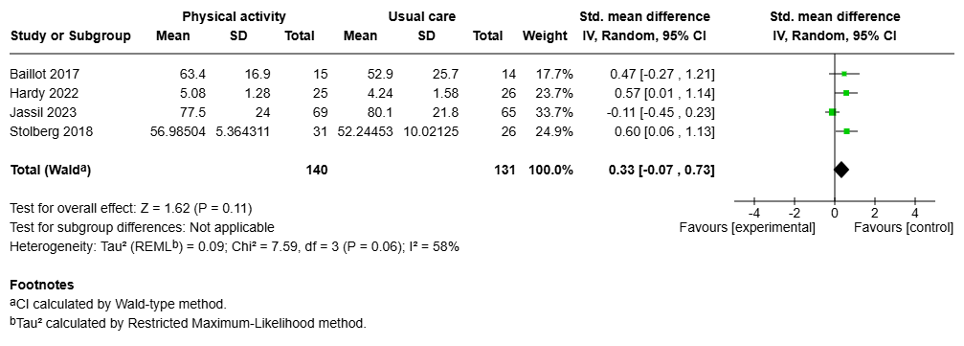
3.3.Social domain
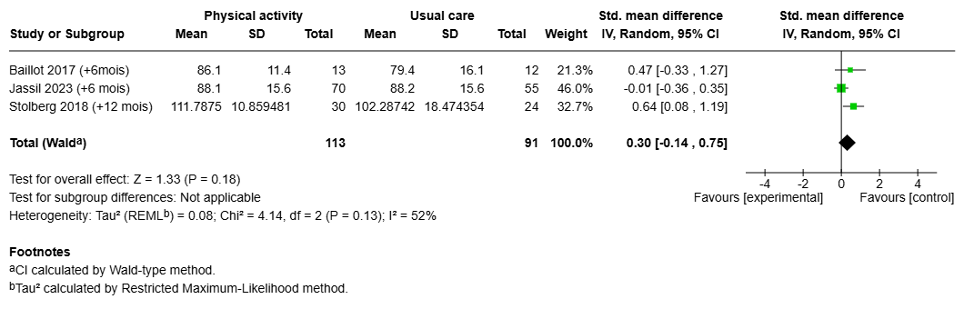
4.Overall delayed analysis
5.Meta-analysis results
BIBLIOGRAPHY
- Obesity and overweight [Internet]. [cité 6 janv 2025]. Disponible sur: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Phelps NH, Singleton RK, Zhou B, Heap RA, Mishra A, Bennett JE, et al. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. The Lancet. 16 mars 2024;403(10431):1027‑50.
- Almeda-Valdes P, Aguilar-Salinas CA, Uribe M, Canizales-Quinteros S, Méndez-Sánchez N. Impact of anthropometric cut-off values in determining the prevalence of metabolic alterations. Eur J Clin Invest. 2016;46(11):940‑6.
- Hendren NS, de Lemos JA, Ayers C, Das SR, Rao A, Carter S, et al. Association of Body Mass Index and Age With Morbidity and Mortality in Patients Hospitalized With COVID-19. Circulation. 12 janv 2021;143(2):135‑44.
- Hutten CG, Padalia K, Vasbinder A, Huang Y, Ismail A, Pizzo I, et al. Obesity, Inflammation, and Clinical Outcomes in COVID-19: A Multicenter Prospective Cohort Study. J Clin Endocrinol Metab. 15 oct 2024;109(11):2745‑53.
- Ioannou GN, Weiss NS, Kowdley KV, Dominitz JA. Is obesity a risk factor for cirrhosis-related death or hospitalization? a population-based cohort study. Gastroenterology. 1 oct 2003;125(4):1053‑9.
- Zhang H, Zhou XD, Shapiro MD, Lip GYH, Tilg H, Valenti L, et al. Global burden of metabolic diseases, 1990–2021. Metab – Clin Exp [Internet]. 1 nov 2024 [cité 15 janv 2025];160. Disponible sur: https://www.metabolismjournal.com/article/S0026-0495(24)00226-9/abstract
- Zhang X, Liu J, Ni Y, Yi C, Fang Y, Ning Q, et al. Global Prevalence of Overweight and Obesity in Children and Adolescents. JAMA Pediatr. août 2024;178(8):800‑13.
- World Obesity Federation Global Obesity Observatory [Internet]. [cité 15 janv 2025]. World Obesity Day Atlases | Obesity Atlas 2024. Disponible sur: https://data.worldobesity.org/publications/?cat=22
- Okunogbe A, Nugent R, Spencer G, Powis J, Ralston J, Wilding J. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob Health. sept 2022;7(9):e009773.
- Jeon E, Lee KY, Kim KK. Approved Anti-Obesity Medications in 2022 KSSO Guidelines and the Promise of Phase 3 Clinical Trials: Anti-Obesity Drugs in the Sky and on the Horizon. J Obes Metab Syndr. 30 juin 2023;32(2):106‑20.
- De Luca M, Belluzzi A, Salminen P, Bueter M, Pujol-Rafols J, Sakran N, et al. Development of the International Federation for Surgery of Obesity and Metabolic Disorders-European Chapter (IFSO-EC) Grade-Based Guidelines on the Surgical Treatment of Obesity Using Multimodal Strategies: Design and Methodological Aspects. J Clin Med. 28 août 2024;13(17):5106.
- Haute Autorité de Santé – Obésité de l’adulte : prise en charge de 2e et 3e niveaux [Internet]. [cité 15 avr 2025]. Disponible sur: https://www.has-sante.fr/jcms/p_3346001/fr/obesite-de-l-adulte-prise-en-charge-de-2e-et-3e-niveaux
- Carrano FM, Iossa A, Di Lorenzo N, Silecchia G, Kontouli KM, Mavridis D, et al. EAES rapid guideline: systematic review, network meta-analysis, CINeMA and GRADE assessment, and European consensus on bariatric surgery-extension 2022. Surg Endosc Interv Tech. mars 2022;36(3):1709‑25.
- Lei Y, Lei X, Chen G, Wang Z, Song H, Feng X, et al. Update on comparison of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass: a systematic review and meta-analysis of weight loss, comorbidities, and quality of life at 5 years. BMC Surg. 30 juill 2024;24(1):219.
- O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss at 10 or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. janv 2019;29(1):3‑14.
- Arterburn D, Wellman R, Emiliano A, Smith SR, Odegaard AO, Murali S, et al. Comparative Effectiveness and Safety of Bariatric Procedures for Weight Loss: A PCORnet Cohort Study. Ann Intern Med. 4 déc 2018;169(11):741‑50.
- Rubino F, Nathan DM, Eckel RH, Schauer PR, Alberti KGMM, Zimmet PZ, et al. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Diabetes Care. juin 2016;39(6):861‑77.
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg. oct 2015;25(10):1822‑32.
- Brown WA, Liem R, Al-Sabah S, Anvari M, Boza C, Cohen RV, et al. Metabolic Bariatric Surgery Across the IFSO Chapters: Key Insights on the Baseline Patient Demographics, Procedure Types, and Mortality from the Eighth IFSO Global Registry Report. Obes Surg. mai 2024;34(5):1764‑77.
- Salem L, Jensen CC, Flum DR. Are bariatric surgical outcomes worth their cost? A systematic review. J Am Coll Surg. févr 2005;200(2):270.
- Haute Autorité de Santé [Internet]. [cité 15 avr 2025]. Guide du parcours de soins : surpoids et obésité de l’adulte. Disponible sur: https://www.has-sante.fr/jcms/p_3408871/fr/guide-du-parcours-de-soins-surpoids-et-obesite-de-l-adulte
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet Lond Engl. 21 juill 2012;380(9838):219‑29.
- Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J Psychiatr Res. juin 2016;77:42‑51.
- Leemans G, Taeymans J, Van Royen P, Vissers D. Respiratory physiotherapy interventions focused on exercise training and enhancing physical activity levels in people with chronic obstructive pulmonary disease are likely to be cost-effective: a systematic review. J Physiother. oct 2021;67(4):271‑83.
- Haute Autorité de Santé [Internet]. [cité 15 avr 2025]. Consultation et prescription médicale d’activité physique à des fins de santé. Disponible sur: https://www.has-sante.fr/jcms/c_2876862/fr/consultation-et-prescription-medicale-d-activite-physique-a-des-fins-de-sante
- Article – Bulletin épidémiologique hebdomadaire [Internet]. [cité 15 avr 2025]. Disponible sur: https://beh.santepubliquefrance.fr/beh/2020/HS/2020_HS_7.html
- Dawes AJ, Maggard-Gibbons M, Maher AR, Booth MJ, Miake-Lye I, Beroes JM, et al. Mental Health Conditions Among Patients Seeking and Undergoing Bariatric Surgery: A Meta-analysis. JAMA. 12 janv 2016;315(2):150‑63.
- Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association Between Physical Activity and Risk of Depression: A Systematic Review and Meta-analysis. JAMA Psychiatry. 1 juin 2022;79(6):550‑9.
- Walfish S, Vance D, Fabricatore AN. Psychological evaluation of bariatric surgery applicants: procedures and reasons for delay or denial of surgery. Obes Surg. déc 2007;17(12):1578‑83.
- Stewart F, Avenell A. Behavioural Interventions for Severe Obesity Before and/or After Bariatric Surgery: a Systematic Review and Meta-analysis. Obes Surg. juin 2016;26(6):1203‑14.
- Bellicha A, Ciangura C, Poitou C, Portero P, Oppert JM. Effectiveness of exercise training after bariatric surgery-a systematic literature review and meta-analysis. Obes Rev Off J Int Assoc Study Obes. nov 2018;19(11):1544‑56.
- Bellicha A, Van Baak MA, Battista F, Beaulieu K, Blundell JE, Busetto L, et al. Effect of exercise training before and after bariatric surgery: A systematic review and meta‐analysis. Obes Rev. juill 2021;22(S4):e13296.
- Stewart F, Avenell A. Behavioural Interventions for Severe Obesity Before and/or After Bariatric Surgery: a Systematic Review and Meta-analysis. Obes Surg. juin 2016;26(6):1203‑14.
- Marshall S, Mackay H, Matthews C, Maimone IR, Isenring E. Does intensive multidisciplinary intervention for adults who elect bariatric surgery improve post-operative weight loss, co-morbidities, and quality of life? A systematic review and meta-analysis. Obes Rev Off J Int Assoc Study Obes. juill 2020;21(7):e13012.
- Baillot A, Romain AJ, Boisvert-Vigneault K, Audet M, Baillargeon JP, Dionne IJ, et al. Effects of lifestyle interventions that include a physical activity component in class II and III obese individuals: a systematic review and meta-analysis. PloS One. 2015;10(4):e0119017.
- Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 4 oct 2016;4:2050312116671725.
- Stolberg CR, Mundbjerg LH, Bladbjerg EM, Funch-Jensen P, Gram B, Juhl CB. Physical training following gastric bypass: effects on physical activity and quality of life-a randomized controlled trial. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. déc 2018;27(12):3113‑22.
- Jassil FC, Carnemolla A, Kingett H, Doyle J, Kirk A, Lewis N, et al. Impact of nutritional-behavioral and supervised exercise intervention following bariatric surgery: The BARI-LIFESTYLE randomized controlled trial. Obes Silver Spring Md. août 2023;31(8):2031‑42.
- Hardy K, Kwok K, Bouchard DR, Bharti N, Gamey D, Vergis A. Impact of a Preoperative Exercise Program on General Fitness in Patients Awaiting Bariatric Surgery: A Pilot Randomized Trial. Cureus. févr 2022;14(2):e22566.
- Baillot A, Vallée CA, Mampuya WM, Dionne IJ, Comeau E, Méziat-Burdin A, et al. Effects of a Pre-surgery Supervised Exercise Training 1 Year After Bariatric Surgery: a Randomized Controlled Study. Obes Surg. avr 2018;28(4):955‑62.
- Arman N, Tokgoz G, Seyit H, Karabulut M. The effects of core stabilization exercise program in obese people awaiting bariatric surgery: A randomized controlled study. Complement Ther Clin Pract. mai 2021;43:101342.
- Bond DS, Thomas JG, King WC, Vithiananthan S, Trautvetter J, Unick JL, et al. Exercise improves quality of life in bariatric surgery candidates: results from the Bari-Active trial. Obes Silver Spring Md. mars 2015;23(3):536‑42.
- Sellberg F, Possmark S, Willmer M, Tynelius P, Berglind D. One-year follow-up of a dissonance-based intervention on quality of life, wellbeing, and physical activity after Roux-en-Y gastric bypass surgery: a randomized controlled trial. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. oct 2019;15(10):1731‑7.